Beagle Obesity How to Monitor Progress Safely

Obesity monitoring and surveillance - what is being done?
Obesity-specific surveys
The WHO European Childhood Obesity Surveillance Initiative(COSI) is an initiative that has measured trends in overweight and obesity in primary school-aged children for over 10 years. The initiative is an example of both obesity-specific monitoring and surveillance and one that is standardised across countries.
Another example of obesity-specific surveys includes the many one-off studies completed by researchers who measure overweight and obesity within set populations. While these studies often are one-offs, they play an important role in providing us with a snapshot of the situation, particularly when national surveys are absent.
National health surveys
Many countries also conduct regular, national health surveys. An example of this is in Mexico, where a flagship National Health and Nutrition Survey (Encuesta Nacional de Salud y Nutricin) is conducted approximately every two years. This survey collates prevalence and trend data (broken down by population) on several different indicators of health and nutrition including overweight and obesity. The survey uses large, nationally representative samples, and the results are based on measured weight and heights.
New Zealand has a similar monitoring programme in place. In both of these examples, standardised methodologies are used each time with appropriately trained personnel. The use of the same methodology over regular time intervals allows the collection of useful trend data.
Bookshelf
Learning Outcome
Recall the causes of obesity
Define BMI and its classification
Summarize the complications of obesity
Describe the role of the nurse in the management of an obese patient
Introduction
Obesity is the excessive or abnormal accumulation of fat or adipose tissue in the body that may impair health. Obesity has become an epidemic which hasworsened for the last 50 years. In the United States, the economic burden is estimated to be about $100 billion annually. Obesity is a complex disease and has multifactorial etiology. It is the second most common cause of preventable death after smoking. Obesity is associated with multiple medical conditions and can cause serious complications of chronic conditions. Obesityneeds multiprong treatment strategies and may require lifelong treatment. A 5% to 10% weight loss can significantly improve health, quality of life, and economic burden of an individual and a country as a whole.[1][2][3][4][5]
Nursing Diagnosis
Imbalance in nutrition
Social isolation
Altered body image
Lack of exercise
Over eating
Poor dietary habits
Depression
Anxiety
Causes
Obesity is the result of an imbalance between daily energy intake and energy expenditure resulting in excessive weight gain. Obesity is caused by multiple factors which can be genetic, cultural, and societal can be considered common. Other causes of obesity include reduced physical activity, insomnia, food habits, endocrine disorders, medications, food advertisements, and energy metabolism.
Most common syndromes associated with obesity include Prader Willi syndrome and MC4Rsyndromes, others like fragile X, Bardet-Beidl syndrome, Wilson Turner congenital leptin deficiency, and Alstrom syndromeare also associated with obesity.
Risk Factors
Nearly one-thirdof adults and about 17% of adolescents in the UnitedStates are obese. According to Center for Disease Control and Prevention (CDC), 2011 to 2012 data, one out of five adolescents, one out of six elementary school age children, and one out of 12 preschool age children are obese. Obesity is more prevalent in African Americans, followed by Hispanics and whites. Southern US states have the highest prevalence, followed by the Midwest, Northeast and the west.
Assessment
All children six years and older, adolescents, and all adults should be screened for obesity according to the United States PreventativeServices Task Force (USPSTF) recommendations.
Physicians should carefully screenfor underlying causes contributing to obesity. A complete history should include:
Childhood weight history
Prior weight loss efforts and results
Complete nutrition history
Sleep patterns
Physical activity
Associated past medical histories like cardiovascular, diabetes, thyroid, and depression
Surgical history
Medications which can promote weight gain
Social histories of tobacco and alcohol use
Family history
Complete Physical examination Should be done and should include body mass index (BMI) measurement, weight circumference, body habitus, vitals.
Obesity focus findings like acne, hirsutism, skin tags, acanthosis nigricans, striae, Mallampati scoring, buffalo hump, fat pad distribution, irregular rhythms, gynecomastia, abdominal pannus, hepatosplenomegaly, hernias, hypoventilation, pedal edema, varicoceles, stasis dermatitis, and gait abnormalities can be present.
Evaluation
A standard screening tool for obesity is the measurement of body mass index (BMI). BMI is calculated using weight in kilograms divided by the square of height in meters.[6][7][8][9][10]Obesity can be classified according to BMI:
Underweight: less than 18.5 kg/m2
Normal range: 18.5kg/m2to 24.9 kg/m2
Overweight: 25kg/m2to 29.9 kg/m2
Obese, Class I: 30 kg/m2 to 34.9 kg/m2
Obese, Class II: 35 kg/m2 to 39.9 kg/m2
Obese, Class III: more than 40 kg/m2
Waist to hip ratio should be measured, in men more than 1:1 and women more than 0:8 is considered significant.
Further evaluation studies like skinfold thickness, bioelectric impedance analysis, CT, MRI, DEXA, water displacement, and air densitometry studies can be done.
Laboratory studies include complete blood picture, basic metabolic panel, renal function, liver function study, lipid profile, HbA1C, TSH, vitamin D levels, urinalysis, CRP, other studies like ECG and sleep studies can be done for evaluating associated medical conditions.
Medical Management
Obesity causes multiple comorbid and chronic medical conditions, and physicians should have a multiprong approach in the management of obesity. Practitionersshould individualize treatment, treat underlying secondary causes of obesity, and focus on managing or controlling associated comorbid conditions. Management should include dietary modification, behavior interventions, medications, and surgical intervention if needed.
Dietary modification should be individualized with close monitoring of regular weight loss. Low-calorie diets are recommended. Low calorie could be carbohydrate or fat restricted. A low-carbohydrate diet can produce greater weight loss in the first months compared to low-fat diet. The patient's adherence to theirdiet should frequently be emphasized.
Behavior Interventions: The USPSTF recommends obese patients to be referred to intensive behavior interventions. Several psychotherapeutic interventions are available which includes motivational interviewing, cognitive behavior therapy, dialectical behavior therapy, and interpersonal psychotherapy. Behavior interventions are more effective when they are combined with diet and exercise.
Medications: Antiobesity medications can be used for BMI greater than or equal to 30 or BMI greater than or equal to 27 with comorbidities. Medications can be combined with diet, exercise, and behavior interventions. FDA-approved antiobesity medications include phentermine, orlistat, lorcaserin, liraglutide, diethylpropion, phentermine/topiramate, naltrexone/bupropion, phendimetrazine. All the agents are used for long-term weight management. Orlistat is usually the first choice because of its lack of systemic effects due to limited absorption. Lorcaserin should be avoided with other serotonergic medications due to the risk of serotonin syndrome. High responders usually lose more than 5% weight in first three months.
Surgery: Indications for surgery are a BMI greater or equal to 40 or a BMI of 35 or greater with severe comorbid conditions. The patient should be compliant with post-surgery lifestyle changes, office visits, and exercise programs. Patients should have an extensive preoperative evaluation of surgical risks. Commonly performed bariatric surgeries include adjustable gastric banding, Rou-en-Y gastric bypass, and sleeve gastrectomy. Rapid weight loss can be achieved with gastric bypass, and it is the most commonly performed procedure. Early postoperative complications include leak, infection, postoperative bleeding, thrombosis, cardiac events. Late complications include malabsorption, vitamin and mineral deficiency, refeeding syndrome, dumping syndrome.[11][12][13]
Nursing Management
Review risk factors for obesity in the patient
Encourage healthy eating
Encourage exercise
Educate patients about the harms of obesity
Enhance self-care and self-esteem
Develop a food diary
Avoid fast foods
Be realistic about weight loss
Eat at scheduled times
Slowly cut down on food portions
Use weight loss drugs with caution
Consider surgery if medical methods fail to help you lose weight
Consult with a dietitian about a healthy diet
Coordination of Care
The management of obesity is best done with a multidisciplinary team that includes a bariatric nurse, surgeon, internist, primary care provider, endocrinologist, and a pharmacist. The key is to educate the patient on the importance of changes in lifestyle. No intervention works if the patient remains sedentary. Even after surgery, some type of exercise program is necessary to prevent weight gain. So far there is no magic bullet to reverse obesity- all treatments have high failure rates and some like surgery also have life-threateningcomplications. Lifestyle changes alone can help obese people reverse the weight gain, but the problem is most people are not motivated to exercise.[13][14]
Health Teaching and Health Promotion
The obesity epidemic is continuing to worsen and has become a public health issue. The management and prevention of obesity is best done with an interprofessional team that includes a bariatric nurse, surgeon, internist, primary care provider, endocrinologist, and a pharmacist. There is no cure for obesity and almost every treatment available has limitations and potential adverse effects.
The key is to educate the patient on the importance of changes in lifestyle. All clinicians who look after obese patients have the onus to educate patients on the harms of the disorders. No intervention works if the patient remains sedentary. Even after surgery, some type of exercise program is necessary to prevent weight gain. So far there is no magic bullet to reverse obesity- all treatments have high failure rates and some like surgery also have life-threateningcomplications. There is an important need for collaboration between the fast-food industry, schools, physical therapists, dietitians, clinicians, and public health authorities to create better and safer eating habits.
Lifestyle changes alone can help obese people reverse the weight gain, but the problem is most people are not motivated to exercise.[13][14]
Pearls and Other issues
Management of obesity should also include prevention strategies with physical activity, exercise, nutrition, and weight maintenance.
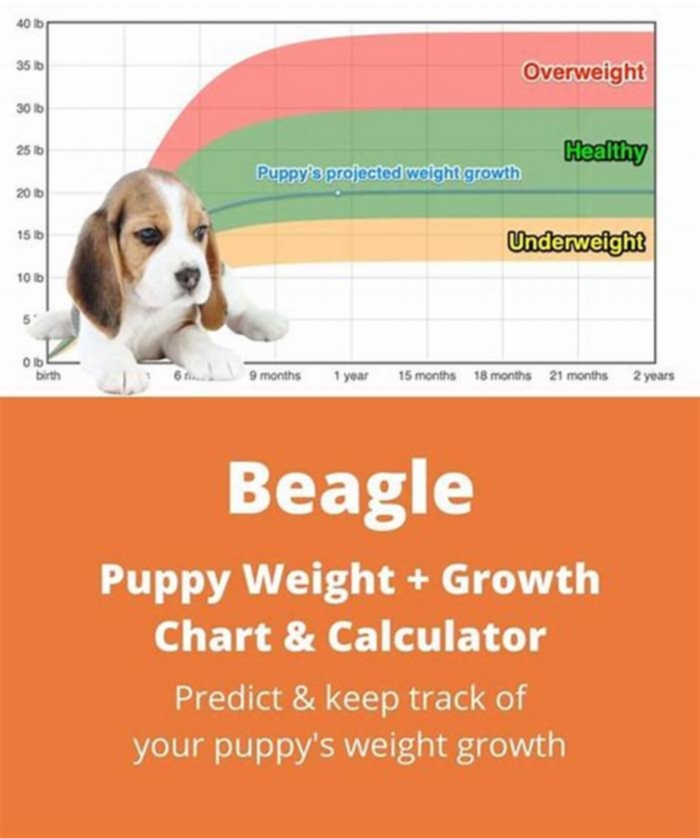
BMI chart with obesity classifications adopted from the WHO 1998 report. Contributed by the World Health Organization - "Report of a WHO consultation on obesity. Obesity Preventing and Managing a Global Epidemic."
References
- 1.
Saalbach A, Anderegg U. Thy-1: more than a marker for mesenchymal stromal cells.
FASEB J. 2019 Jun;33(6):6689-6696.[
PubMed: 30811954]
- 2.
Kozlov AI. [Carbohydrate-related nutritional and genetic risks of obesity for indigenous northerners].
Vopr Pitan. 2019;88(1):5-16.[
PubMed: 30811129]
- 3.
Gowd V, Xie L, Zheng X, Chen W. Dietary fibers as emerging nutritional factors against diabetes: focus on the involvement of gut microbiota.
Crit Rev Biotechnol. 2019 Jun;39(4):524-540.[
PubMed: 30810398]
- 4.
Holly JMP, Biernacka K, Perks CM. Systemic Metabolism, Its Regulators, and Cancer: Past Mistakes and Future Potential.
Front Endocrinol (Lausanne). 2019;10:65.[
PMC free article: PMC6380210] [
PubMed: 30809194]
- 5.
Akinkuotu AC, Hamilton JK, Birken C, Toulany A, Strom M, Noseworthy R, Hagen J, Dettmer E, Langer JC. Evolution and Outcomes of a Canadian Pediatric Bariatric Surgery Program.
J Pediatr Surg. 2019 May;54(5):1049-1053.[
PubMed: 30808540]
- 6.
Desprs JP, Nadeau A, Tremblay A, Ferland M, Moorjani S, Lupien PJ, Thriault G, Pinault S, Bouchard C. Role of deep abdominal fat in the association between regional adipose tissue distribution and glucose tolerance in obese women.
Diabetes. 1989 Mar;38(3):304-9.[
PubMed: 2645187]
- 7.
Fujioka S, Matsuzawa Y, Tokunaga K, Tarui S. Contribution of intra-abdominal fat accumulation to the impairment of glucose and lipid metabolism in human obesity.
Metabolism. 1987 Jan;36(1):54-9.[
PubMed: 3796297]
- 8.
Sparrow D, Borkan GA, Gerzof SG, Wisniewski C, Silbert CK. Relationship of fat distribution to glucose tolerance. Results of computed tomography in male participants of the Normative Aging Study.
Diabetes. 1986 Apr;35(4):411-5.[
PubMed: 3956878]
- 9.
Ruderman NB, Berchtold P, Schneider S. Obesity-associated disorders in normal-weight individuals: some speculations.
Int J Obes. 1982;6 Suppl 1:151-7.[
PubMed: 6749721]
- 10.
Bonora E, Kiechl S, Willeit J, Oberhollenzer F, Egger G, Meigs JB, Bonadonna RC, Muggeo M. Insulin resistance as estimated by homeostasis model assessment predicts incident symptomatic cardiovascular disease in caucasian subjects from the general population: the Bruneck study.
Diabetes Care. 2007 Feb;30(2):318-24.[
PubMed: 17259501]
- 11.
Karelis AD, St-Pierre DH, Conus F, Rabasa-Lhoret R, Poehlman ET. Metabolic and body composition factors in subgroups of obesity: what do we know?
J Clin Endocrinol Metab. 2004 Jun;89(6):2569-75.[
PubMed: 15181025]
- 12.
Ferrante AW. Obesity-induced inflammation: a metabolic dialogue in the language of inflammation.
J Intern Med. 2007 Oct;262(4):408-14.[
PubMed: 17875176]
- 13.
Neels JG, Olefsky JM. Inflamed fat: what starts the fire?
J Clin Invest. 2006 Jan;116(1):33-5.[
PMC free article: PMC1323268] [
PubMed: 16395402]
- 14.
Mercado-Gonzales SI, Carpio-Rodrguez AN, Carrillo-Larco RM, Bernab-Ortiz A. Sleep Duration and Risk of Obesity by Sex: Nine-Year Follow-Up of the Young Lives Study in Peru.
Child Obes. 2019 May/Jun;15(4):237-243.[
PMC free article: PMC7613162] [
PubMed: 30810346]
- 15.
Shiozawa B, Madsen C, Banaag A, Patel A, Koehlmoos T. Body Mass Index Effect on Health Service Utilization Among Active Duty Male United States Army Soldiers.
Mil Med. 2019 Oct 01;184(9-10):447-453.[
PubMed: 30811530]
- 16.
Al-Nimr RI. Optimal Protein Intake during Weight Loss Interventions in Older Adults with Obesity.
J Nutr Gerontol Geriatr. 2019 Jan-Mar;38(1):50-68.[
PubMed: 30806592]
- 17.
Pasarica M, Topping D. An Evidence-Based Approach to Teaching Obesity Management to Medical Students.
MedEdPORTAL. 2017 Dec 20;13:10662.[
PMC free article: PMC6338064] [
PubMed: 30800862]
- 18.
Walsh K, Grech C, Hill K. Health advice and education given to overweight patients by primary care doctors and nurses: A scoping literature review.
Prev Med Rep. 2019 Jun;14:100812.[
PMC free article: PMC6374522] [
PubMed: 30805277]
- 19.
Ball W, Raza SS, Loy J, Riera M, Pattar J, Adjepong S, Rink J. Effectiveness of Intra-Gastric Balloon as a Bridge to Definitive Surgery in the Super Obese.
Obes Surg. 2019 Jun;29(6):1932-1936.[
PubMed: 30806915]
- 20.
Klebanoff MJ, Corey KE, Samur S, Choi JG, Kaplan LM, Chhatwal J, Hur C. Cost-effectiveness Analysis of Bariatric Surgery for Patients With Nonalcoholic Steatohepatitis Cirrhosis.
JAMA Netw Open. 2019 Feb 01;2(2):e190047.[
PMC free article: PMC6484583] [
PubMed: 30794300]
- 21.
Monteiro JLGC, Pellizzer EP, Arajo Lemos CA, de Moraes SLD, do Egito Vasconcelos BC. Is there an association between overweight/obesity and dental implant complications? A systematic review and meta-analysis.
Int J Oral Maxillofac Surg. 2019 Sep;48(9):1241-1249.[
PubMed: 30792086]
- 22.
Barr AC, Lak KL, Helm MC, Kindel TL, Higgins RM, Gould JC. Linear vs. circular-stapled gastrojejunostomy in Roux-en-Y gastric bypass.
Surg Endosc. 2019 Dec;33(12):4098-4101.[
PubMed: 30805785]
Disclosure: Kiran Panuganti declares no relevant financial relationships with ineligible companies.
Disclosure: Minhthao Nguyen declares no relevant financial relationships with ineligible companies.
Disclosure: Ravi Kshirsagar declares no relevant financial relationships with ineligible companies.
Disclosure: Chaddie Doerr declares no relevant financial relationships with ineligible companies.